By Womaness Editors 9-Minute Read

Questions about menopause? Somi Javaid, MD has heard them all. As founder and Chief Medical Officer of HerMD—female-forward wellness centers in the Cincinnati area committed to empowering women through comprehensive health, beauty, and wellness services—the board-certified OBGYN ensures a safe space for women to address any of their needs, no matter how personal. “There should be no stigma or shame,” she explains. “It should be something you can discuss with your health-care provider to find what helps you get back to where you want to be.”
Here, Dr. Javaid gives us a rundown of the top questions she hears from women in menopause…as well as the answers she gives her own patients.
#1. “Why are things changing for me in the bedroom?”
Dr. Javaid: Up until now, menopause was a taboo topic. Women haven't really had a place to discuss or learn about it...so everyone seems to think menopause is limited to hot flashes or sleep problems. A lot of menopausal patients therefore are very curious about the changes also occurring to them within the different domains of sexuality.
Sex means very different things from patient to patient. In our offices, we measure things like libido, arousal, pain, and orgasm and look at all the different aspects of female sexuality. We're a safe space, and we explain that many of the changes patients go through are due to hormonal changes. As you go into menopause, your estrogen levels decline, as do your testosterone levels. A lot of women don't realize that testosterone is just as important for our sexuality as it is for our male counterparts. In fact, in 2019, a global consensus statement came out about the importance of testosterone and how it can help improve all the domains of sexuality. It also examined its safety for women. It looked at topics like, as a side effect of testosterone, are women more likely to have problems with their breasts or have high cholesterol? In the three years they studied women and testosterone, no problems were found. But it’s confusing for women: there are currently no FDA-approved testosterone-only treatment options for them. Everything is compounded, off-label, or a male-only product. I think that (and the not knowing) has created a resistance.
Where did my desire go?
Desire for women is very complex. It involves hormones and neurotransmitters in the brain. There was a very elegant study done on women who have what they described as “normal” desire and on women who were struggling with it. The researchers showed everyone erotica, put them in PET scanners, and observed the neural activity. The women who struggled with desire had very low excitatory levels of neurotransmitter activity and very high inhibitory activity; the women who weren't struggling showed the exact opposite. So we know our brain is what I call “the most important sex organ.” Without it, you can't orgasm and you won't have arousal or desire. Environmental factors are also involved. If you are in a loving relationship where you feel desired and supported, you’re more likely to have desire than you are if you’re not connecting with your partner. There are multiple facets—but when you add the menopause factor with testosterone and estrogen in decline, "I have no desire" becomes a common complaint.
Our brain is what I call “the most important sex organ.”
As a doctor, I have to tease out a few things related to having no desire. Has this been going on for at least six months? Is it distressing to you or is it not where you want it to be? At one point, was your desire what you describe as “normal”? If you meet those criteria and it's not directly attributable to a medication side effect or a health issue, then we call it hypoactive sexual desire disorder (HSDD). I see it in both menopausal patients and pre-menopausal patients. We talk about available medications. If a relationship factor or stress factor is involved, I also send people to counseling.
Why does sex hurt now?
If there's pain involved during sex—which is another common complaint I hear—we call it genitourinary syndrome of menopause (GSM). Our external and internal anatomy are very dependent upon hormones. You know, I compare a normal, healthy vagina to an accordion: it has these deep folds called rugae, it stretches, and it's pink. As you age and lose those hormone levels, that tissue starts to get thinner…and when you try to stretch that tissue with intercourse, it doesn't do it as well. It almost becomes like a tube sock, burning and hurting. That's when women tell me that sex hurts, or they feel dry, or they hurt the day after. And the reason we call it “genitourinary” is because some women present with bladder symptoms at the same time. They might be leaking with a cough, a sneeze, when they're jumping on a trampoline, or even when they're cheering on their children. These changes are all directly related to hormones declining.
We remember moisturizer for our face, hands, and feet. But a lot of women forget about moisturizing sensitive parts like the vagina and vulva.
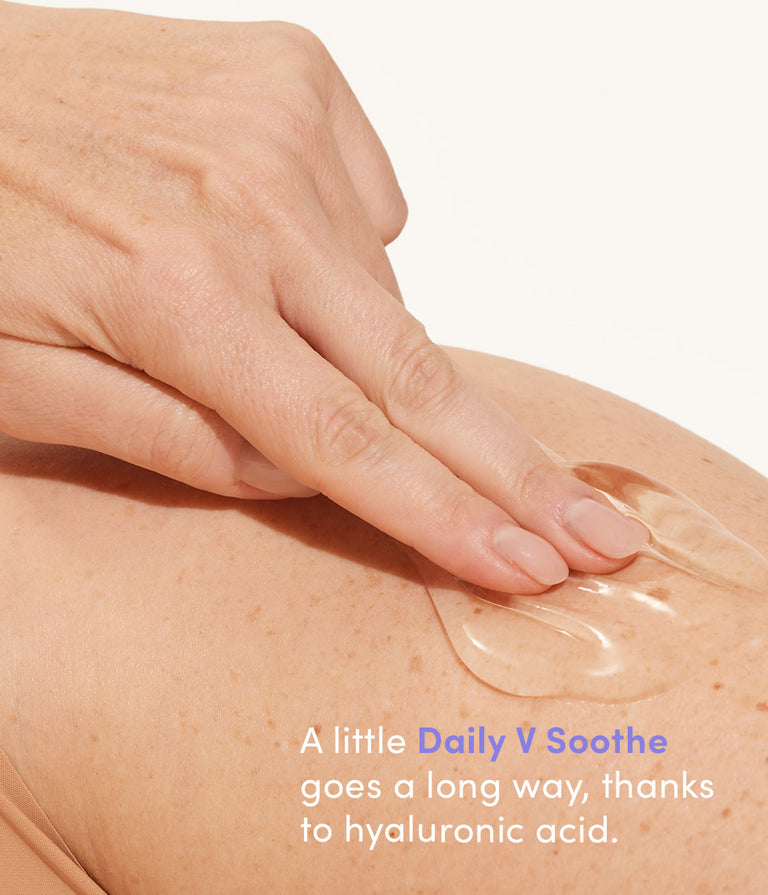
The good news is there are nice treatment options. There are suppositories (usually hormonal) that are locally acting. If you want to avoid that, there's pelvic floor physical therapy. There are surgical options for women having incontinence. There are lasers and radio-frequency treatments for the dryness and pain. There are also great over-the-counter lubricants and moisturizers. We remember moisturizer for our face, hands, and feet. But a lot of women forget about moisturizing sensitive parts like the vagina and vulva. There are now great products out there that can help keep that skin healthy.
Why does my orgasm feel...less than spectacular?
Orgasm complaints are the other question I get. It’s the same thing: Low testosterone levels can affect your ability to orgasm. Orgasm has two parts: It's the physical contractions of your anatomy both internally and externally, and it's that feeling of euphoria. Physically, if your pelvic floor is not as strong as it should be, you may have a muted or dulled orgasm. A pelvic floor helps keep urine and waste in, but it is also those muscles that surround everything in the pelvic girdle that, when relaxed, allows us to have intercourse, undergo a pelvic exam, or insert a tampon. So if there is laxity, I get women in pelvic floor physical therapy, which can help them have a better experience in the bedroom.
#2. “I’m eating and exercising like I’ve always done. Why am I gaining weight?”
Dr. Javaid: This question is asked on almost a daily basis! Here’s how women pose it to me: “I’m doing everything I've always done. I am working out. I'm eating healthy. Nothing has changed except the scale—which keeps going up. What’s happening?"
Menopause and weight gain happens all the time. It doesn’t mean it’s inevitable or that there’s nothing you can do or that you'll just keep gaining weight.
I explain to my patients that menopause can prohibit their behavior from actually giving them the results that they want. As you enter menopause, your level of FSH—what we call the "menopause hormone”—starts to increase because estrogen and testosterone are declining. In fact, there have been studies in mice who’ve been injected with FSH—therefore making them menopausal—and become obese. So there is definitely this fat deposition, or deposits of fat that all of a sudden go in the middle area, the belly..."the middle-age spread" actually has a medical explanation to it. It’s different than putting weight on in the breasts and hip like you might have before menopause.
"The middle-age spread" actually has a medical explanation to it.
Your metabolic rate can also slow down. Due to declining testosterone levels, we can also lose muscle mass. When that happens, lost muscle mass can be replaced with more fat, which is what we see in our menopausal patients.
What can you do to naturally combat the changes that happen in menopause? You might have to step up the exercise and pay more attention to what you're eating. Stay hydrated and keep moving! I'm also a huge fan of intermittent fasting. Basically, it controls your insulin levels, which is healthier for us in the long run. It can lead to decreased risk of diabetes, cardiovascular disease, and also some cancers (because we know high insulin levels over a lifetime can increase the risk of some cancers). Overall, it's a healthy way to live. It's not a fad diet; it's sustainable, which I like. Obviously you should talk to your health-care provider and make sure you can do intermittent fasting along with any medications or health conditions you have. But rather than just telling menopausal patients to eat less and workout more, I found intermittent fasting is a valid, valuable tool.
Also, for some women, getting on hormone replacement therapy (HRT) works, whether it's getting their testosterone levels back to normal levels (or what we call "therapeutic levels") and getting their estrogen back up. Because when you give people back estrogen and testosterone, we see their FSH level start to come down. With just HRT and healthy habits, therefore, a lot of my patients will go back to their normal weight or where they've resided their entire lives. Everyone is very different.
#3. “Why is my brain suddenly so foggy?”
Dr. Javaid: Have you read the latest headlines? It’s so eye opening. There was an article about 900,000 women leaving the workforce in the UK due to menopausal symptoms. To me, it is such a tragedy to lose women in the prime of their lives from our workforce just because they're not comfortable discussing what's happening in their brains, or because perhaps there are other symptoms preventing them from working in the manner they're used to.
I personally take care of a lot of women who say they can no longer function the way they normally do in daily life. They'll say:
-
"I can't find my words, Dr. Javaid. Whether I'm talking to my kids or in a board meeting, it's on the tip of my tongue, but I can't find it."
-
"I went to the pantry with a clear intention of what I want. Then I stand in there and go, 'Why am I here?'"
-
“I can’t find things. Or I’ve misplaced something, like my keys or something I need for a meeting…”
Along with cognitive changes like these, we also see increased levels of depression and increased levels of anxiety—because if you feel like you're not functioning the way you're used to or the way you're expected to, it's distressing. It's not something you're doing wrong. Menopause is just happening.
It's not something you're doing wrong. Menopause is just happening.
There are studies supporting mild cognitive decline during this time. As we start to see hormonal levels going down, we do see symptoms like problems with word-finding and memory. But data reviews show that if we treat women early with hormone replacement therapy—right as they're going into menopause, if they are good candidates—we will see benefit. (There were earlier studies that showed no benefit and some harm with cognitive decline with HRT, but that was when doctors were waiting way too long to start it, like 15 or 20 years into menopause.) So, with HRT, I do see improvements clinically with memory, word-finding, and everyday function. Women will say, "Oh my god, Dr. Javaid, I feel like my brain is firing on all cylinders again!" Then I’ll also see a positive impact on mood. Women do feel better. They tend to seem less anxious. And their confidence is restored.
Disclaimer: This article is intended for informational purposes and is not intended to replace a one-on-one relationship with a physician or medical advice. Womaness strives to share the knowledge and advice from our own network of experts and our own research. We encourage you to make healthcare decisions based in partnership with a qualified healthcare professional.
More Menopause Must-Reads
What's Happening Here? Vaginal Dryness