By Womaness Editors 4-Minute Read

If you’ve ever moisturized your face, put sunscreen on your chest, or used a serum on your neck…you already understand the basic idea behind vaginal skincare. It’s just that nobody gave us permission to talk about it like that.
For decades, anything “down there” got shoved into one of two boxes:
1. “Feminine hygiene” (a euphemism-heavy aisle of fragranced nonsense), or
2. “Sex stuff” (which somehow made everyday discomfort feel like a personal failing).
Meanwhile, real, treatable changes in perimenopause, menopause, and midlife overall—dryness, irritation, burning, pain with sex, urinary symptoms—often went unaddressed. The medical term for this cluster is genitourinary syndrome of menopause (GSM), and it’s common, underdiagnosed, and very manageable.
So yes: vaginal skincare is real. And it’s not about vanity. It’s about comfort, confidence, and caring for tissue that changes with hormones—just like the rest of your skin.
“It’s about comfort, confidence, and caring for tissue that changes with hormones—just like the rest of your skin.”
First: what we mean by “vaginal skincare”
When we say vaginal skincare, we mean evidence-based care for the vulva and vagina that supports comfort, moisture, and tissue health—especially in perimenopause and menopause.
That can include:
-
Gentle cleansing habits that protect sensitive tissue (and don’t strip or irritate it)
-
Moisture support (often with non-hormonal vaginal moisturizers used regularly)
-
Lubrication for friction with sex (or pelvic exams—yes, those count)
-
Medical options for moderate to severe symptoms (like prescription local estrogen or other therapies), when appropriate
What vaginal skincare is not
Let’s retire a few myths:
° It’s not douching. (Actually: please don’t. It can irritate and disrupt the vaginal environment.) The American College of Obstetricians & Gynecologists (ACOG) is very clear that the vagina doesn’t need internal “cleaning.”
° It’s not perfumed sprays, scented washes, or harsh antiseptics.
° It’s not trying to make your vagina “smell like a flower.” (A vagina smells like a vagina. That’s the point.)
Quick anatomy refresher (because it matters)
People often say “vagina” when they mean “vulva.”
-
Vulva = the external anatomy (labia, clitoris, vestibule, vaginal opening).
-
Vagina = the internal canal.
Why this matters: products are not one-size-fits-all. Some are designed for external vulvar comfort; others are formulated for internal vaginal tissue. If you’ve ever used the wrong thing in the wrong place and regretted it immediately…welcome to the club.
Why vaginal skincare becomes a thing in midlife
Hormones—especially estrogen—help keep vaginal tissue:
-
supple
-
elastic
-
well-lubricated
-
resilient
As estrogen declines in perimenopause and menopause, the tissue can become drier and more fragile, and vaginal pH can change. Symptoms can include dryness, burning, irritation, pain with sex, and urinary complaints (like urgency or recurrent UTIs). This broader set of changes is what clinicians refer to as GSM.
And here’s the kicker: GSM isn’t rare. The 2020 position statement from The Menopause Society notes it affects a substantial portion of postmenopausal women (estimates vary widely), and it can meaningfully impact quality of life—yet it’s often underreported and undertreated.
In plain English: this is common, treatable, and not something you should silently push through.
The 3 most useful categories of vaginal care products
Not all vaginal products do the same job...and understanding the difference matters. Most clinicians think about vaginal care in layers, depending on symptoms, severity, and goals.
1) Lubricants (for friction, right now)
Lubricants are designed to reduce friction during sex or any penetrative activity (including pelvic exams). They’re used as needed, and their benefits stop when the activity does.
They’re helpful—but they don’t treat underlying dryness or tissue changes. Many experts recommend choosing products that are as “body-similar” as possible, paying attention to factors like pH and osmolality, which can affect irritation risk.
2) Vaginal moisturizers (for ongoing surface hydration)
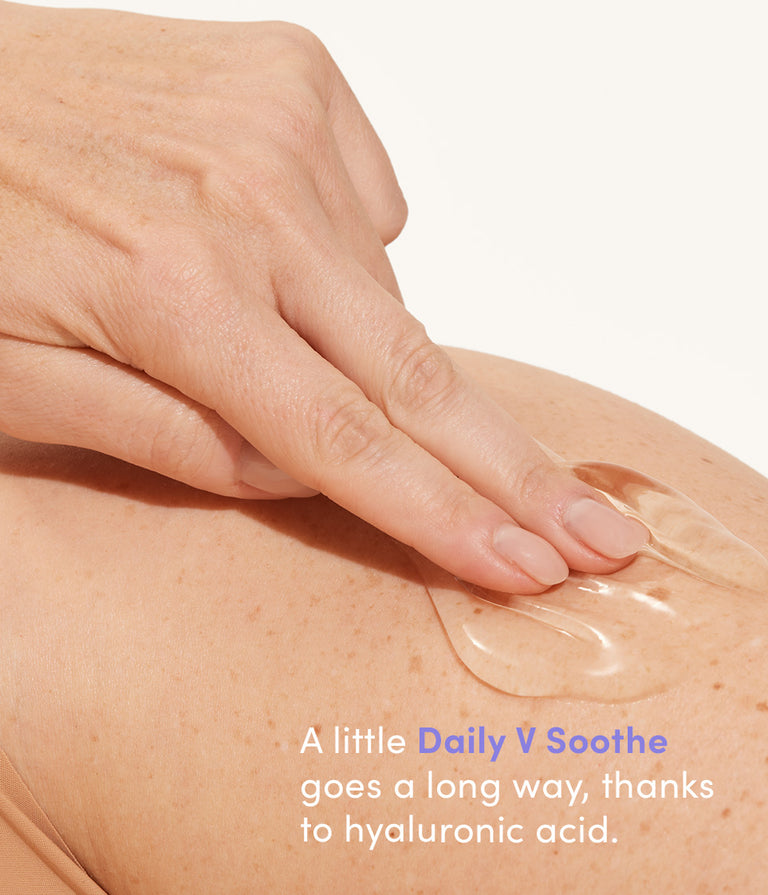
While they can also work to prep you for intimacy like a lubricant, vaginal moisturizers are intended for regular use, independent of sexual activity. They help replenish moisture, improve comfort, and support vaginal tissue over time—especially for women experiencing day-to-day dryness, itching, or irritation.
Because they’re used consistently (often several times per week), moisturizers tend to offer more sustained relief than lubricants alone. Both ACOG and menopause-focused clinical guidance recognize non-hormonal vaginal moisturizers as a first-line option for mild to moderate symptoms.
3) Vaginal suppositories and inserts (for deeper, longer-lasting support)
Vaginal suppositories—sometimes called inserts—are designed to deliver hydration or therapeutic ingredients internally, where estrogen-related tissue changes are most pronounced.
Nonhormonal suppositories are often used when:
-
dryness is persistent or more noticeable internally
-
surface moisturizers aren’t quite enough
-
symptoms affect comfort during daily life or intimacy
Depending on formulation, suppositories may be used on a scheduled basis (for example, several times per week) to provide even more intensive, longer-lasting moisture support. Some non-hormonal formulations—such as those containing hyaluronic acid—have been studied for their ability to improve vaginal dryness symptoms in postmenopausal women.
For moderate to severe symptoms of genitourinary syndrome of menopause (GSM), prescription therapies (including local vaginal estrogen and other clinician-directed options) may be appropriate, depending on your health history and preferences. Clinical guidelines emphasize a step-up approach that matches treatment intensity to symptom severity.
A note on hyaluronic acid (because you’ll see it everywhere)
Hyaluronic acid (HA) is a well-known hydrating ingredient in facial skincare—and it also shows up in research on nonhormonal approaches for vaginal dryness and GSM symptoms.
Recent and past studies have examined HA-based vaginal products in postmenopausal populations, including comparisons with local estrogen therapies. Results vary by study design and endpoints, but overall the evidence supports HA as a reasonable nonhormonal option for symptom relief for some women.
Important nuance: local estrogen does often perform better on certain objective tissue findings in moderate-to-severe GSM, and some guidelines still place it as a highly effective option when indicated.
Translation: non-hormonal options can help a lot—AND there are times when prescription therapy is the right call.
“When we say vaginal skincare, we mean evidence-based care for the vulva and vagina that supports comfort, moisture, and tissue health—especially in perimenopause and menopause.”
So, why didn’t anyone tell us sooner?
Because women’s health has a long history of being treated as:
-
embarrassing
-
secondary
-
“just part of aging”
But here’s the truth: discomfort isn’t a personality trait. And “fine” shouldn’t mean “silently tolerating dryness and pain.”
Vaginal skincare is simply the grown-up, medically grounded way to talk about something women have been dealing with for years—often alone. And at Womaness? We’re done with that.
Get More Answers
Ask an OB/GYN: "Should I try HRT in perimenopause?"
Ask an OB/GYN: "Can I use vaginal moisturizer with vaginal estrogen?"
Ask a Doctor: "Why does sex hurt now?"