By Julia Walker, RN, BSN 5-Minute Read
Julia Walker, RN, BSN is a women's health nurse, writer, and member of the perry team. Perry connects and supports perimenopause warriors in a safe space to build friendships, learn, and laugh. The moment you think, “WTF, could this be menopause?”—join our sisterhood!
Of all the stages of menopause, perimenopause is perhaps the most murky, varied, and unpredictable. There’s often a lot of misunderstanding and misinformation around the “peri” period as well. Below, we compile all you need to know so that you're well prepared to handle (and thrive) during this bumpy start to menopause.
What is perimenopause?
Translating to “around menopause,” perimenopause is the time your body makes the transition to menopause, marking the end of the reproductive years. It is a bit of a wild, bumpy ride. That’s due to the fact your levels of estrogen are rising and falling, setting the stage for possible hot flashes, sleep issues, and vaginal dryness. Symptoms often start gradually and then tend to ramp up as you get closer to reaching menopause. Some women scrape by with few symptoms; others find their worlds completely rocked by the physical and mental changes they undergo.
When do women enter perimenopause?
Perimenopause is not like clockwork. Women enter into this stage at different ages. Some notice signs such as menstrual irregularity or other perimenopause-like changes as early as their mid- to late-thirties. For most women, the progression starts somewhere in their 40s. Other factors can affect this, from hereditary factors to use of oral contraceptives to lifestyle factors like alcohol consumption, exercise habits, and medical history.
What are the typical symptoms?
The experience for women in perimenopause is anything but typical. For some women, it feels as if they're in the throes of menopause, with the entire platter of issues from hot flashes and night sweats to brain fog to massive mood swings and vaginal dryness to a sexual slump. More subtle changes can range from fluctuations in cholesterol levels to loss of bone density to decreased fertility.
During this period, women can also experience weight gain (mainly around the middle), incontinence, drier skin and hair, brittle nails, hair loss, anxiety, muscle aches, stronger PMS symptoms, breast tenderness, bloating and gas, and increased fatigue after exercise.
Perimenopause can even cause bizarre symptoms to emerge, such as
● Changes in body odor
● Increased allergies
● Dental problems like burning gums
● Muscle aches and pains
● Tingling extremities
● Itching skin
● Electric shocks and vibrations
If you are ever concerned about any symptoms, be sure to connect with your doctor. Feeling anxious about a new development often exacerbates whatever you're experiencing.
“The experience for women in perimenopause is anything but typical.”
So can you still get pregnant in perimenopause?
Absolutely—though your fertility gradually declines in your 30s. (A healthy, fertile 30-year-old woman has a 20% chance of getting pregnant. By age 40, it is less than 5%, and by 45, that number drops to 1%.) While the chances are low, you can still conceive until you have gone a full year (12 consecutive months) without a period.
If you do not wish to become pregnant and are sexually active with a male partner, you will want to use some form of birth control until your doctor gives you the all-clear. They can to discuss various options with you. And don't be surprised if hormonal birth control pills gets mentioned; as it turns out, the consistency of the hormones in the Pill can often help curb perimenopause symptoms for many women. (Indeed, some women taking them say they "glide" through perimenopause more smoothly.)
That said, hormonal birth control is not for everyone. Some women do not feel good on it while others can't take it due to health conditions. Again, a conversation with your doctor is the first place to start when preventing pregnancy in perimenopause.
“You do not officially enter menopause until you have gone a full year without a menstrual cycle.”
When is perimenopause over?
You do not officially enter menopause until you have gone a full year (12 months) without a menstrual cycle. After this, you have entered menopause.
The kicker, though, is that the duration of perimenopause varies from woman to woman. Some will only experience symptoms for a year or two before they're officially in menopause; others will have symptoms for nearly a decade. There's no apparent reason for the variation, but if you want to know what your experience may be like, chat with any women in your family for an idea of how perimenopause was for them and when they officially reached menopause.
So, what's the good news?
Perimenopause is an entirely natural change in your body. Sure, it can be highly disruptive, but it is not a medical condition. And it certainly doesn't require treatment. But that said, there are plenty of ways to manage the different perimenopause symptoms so they don't interfere with your quality of life.
First and foremost, it's crucial to optimize your overall health. Eating a healthy, plant-forward diet and ensuring you get proper exercise is vital.
These easy modifications can also make a big difference:
● Managing stress and caring for your sleep is essential
● Using a vaginal moisturizer can soothe vaginal dryness and serve as a lubricant for less painful sex.
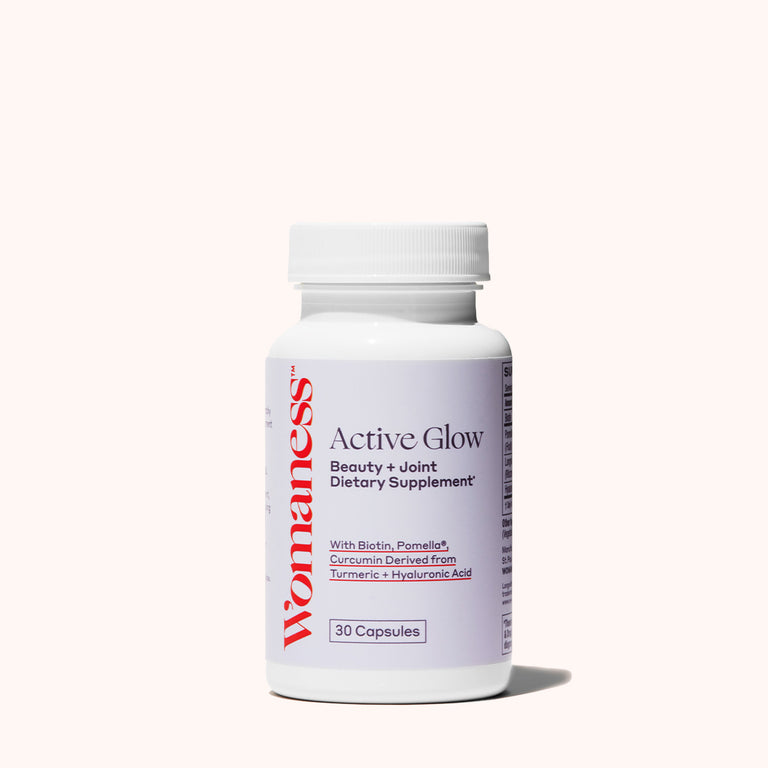
● Treating dry skin, hair, and nails to beneficial, ultra-hydrating ingredients such as hyaluronic acid and biotin.
● Having a cooling spray or body wipes on hand can help manage the heat and perspiration of hot flashes and night sweats.
● Wearing discreet liners can save you from any leaks that accompany a sneeze or a good laugh.
Arming yourself with information about the menopause transition and creating a good relationship with your health care provider can make this transition smoother. Your doctor can advise you on other options for managing your symptoms, including hormone replacement therapy, hormonal birth control pills, supplements, and alternative treatment options. Aside from symptom management, your doctor should be able to set you up with a smart plan for keeping your whole body healthy in perimenopause and beyond—including ways to help ward off osteoporosis and cardiovascular disease, those chronic diseases that notoriously afflict women in the last stage of menopause: postmenopause.
More Perimenopause
Surprising Symptoms, Real Solutions
Top Menopause Myths: Dr. Ekta Kapoor
The Stages of Menopause